Preterm nutrition products
Benefits of an Exclusive Human Milk Diet (EHMD)
More than 20 clinical studies with more than 5,000 premature infants have demonstrated the effectiveness of Prolacta’s 100% human milk-based nutritional products.1
Our products, as part of an exclusive human milk diet, have been shown in clinical studies to:
Our products
Prolacta’s human milk-based nutritional products contain a wide range of human milk oligosaccharides (HMOs) – special sugars abundantly found in human milk.9 HMOs promote the development and maturation of the newborn immune system and provide a supplementary source of sialic acid critical for brain development. 10,11
Humavant+
Humavant+ is the first commercially available human milk fortifier made from 100% human milk.

HumavantTM CR Human Milk Caloric Fortifier
Human milk caloric fortifier is ideal for neonatal infants receiving low caloric content. Data show that 65% of the time, term mother’s own milk (MOM) is less than 20 Cal/30 ml.12 Humavant CR human milk caloric fortifier can meet the need for additional calories.
- Intended for use with MOM or donor milk (DM) to increase lipids and achieve adequate growth
- Formulated to deliver at least 2.6 Cal/ml
- Available frozen in 30 ml bottles containing 10 ml of product
(4 bottles per unit carton, with 48-hour expiration) - Includes simplified preparation instructions
- Easy to use and measure


Humavant CR human milk caloric fortifier is the only completely human solution created to add calories to MOM or DM without substantially increasing volume and without introducing a non-human milk-based nutritional product.
A randomised clinical trial found that premature infants, who received an exclusive human milk diet (EHMD) with Humavant CR fortifier, had superior length and weight velocity compared to infants who received an EHMD without Humavant CR fortifier.13

This study is a subset analysis of data originally published in 2014 by Hair et al in The Journal of Pediatrics.
Clinical Studies and Publications:
- Randomised Trial of Human Milk Cream as a Supplement to Standard Fortification of an Exclusive Human Milk-Based Diet in Infants 750-1,250 g Birth Weight
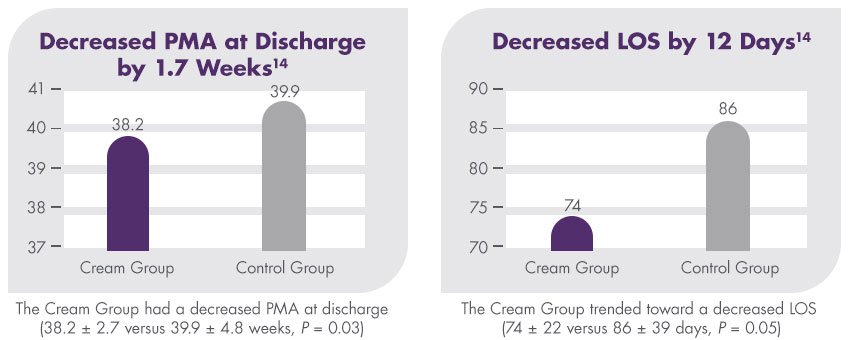
- Premature Infants 750–1,250g Birth Weight Supplemented with a Novel Human Milk-Derived Cream Are Discharged Sooner
- Fortifier and Cream Improve Fat Delivery in Continuous Enteral Infant Feeding of Breast Milk
- Macronutrient analysis of a nationwide sample of donor breast milk
Product information downloads
Overcoming complications
Prolacta’s products, when used as part of an exclusive human milk diet, have been shown to reduce the incidence of clinical complications.
In a multicentre, retrospective cohort study with 1,587 patients, the outcomes of extremely premature infants (< 1,250 g birthweight) who received a diet including cow’s milk-based products were compared with infants who received an EHMD. The incidence of mortality, necrotising enterocolitis (NEC), bronchopulmonary dysplasia (BPD), retinopathy of prematurity (ROP) and late-onset sepsis were all reduced with an EHMD.13

Improving outcomes with Prolacta's exclusive human milk diet
- Decreasing feeding intolerance – Prolacta's EHMD was associated with a lower incidence of feeding intolerance and shorter time to full feeds compared to a diet containing cow milk-based products2
- Supporting adequate growth – An EHMD feeding protocol for infants with a birthweight of ≤1250 g that enables early and rapid fortification advancement is associated with weight, length and head circumference gains meeting targeted standards, and with a low rate of extrauterine growth restriction6,7,13
- Turning to nutrition to address the complications of prematurity – Today, more and more hospitals are turning to Prolacta’s fortifiers that are clinically proven as part of an EHMD; this nutritional solution is shown in a growing body of evidence to reduce the most serious complications of prematurity2,7,14,16

Reducing hospital costs with an EHMD
Very low birthweight babies are at risk for prematurity-related morbidities and interventions, such as BPD, ROP, late-onset sepsis and NEC. The incremental cost of these morbidities and interventions can substantially increase the cost of NICU hospitalisation.


